Vinson Health Center Medical Director gives information on COVID-19
As of March 11, America has confirmed an upwards of 1,300 cases of COVID-19, also known as the Coronavirus. Some 70 of these cases were respirated from overseas while the other cases were detected and confirmed on U.S. soil. The Vinson Health Center Medical Director and Incident Commander of the Incident Management Team Keith Williamson gave more information about COVID-19.
Q: Have there been any confirmed cases in Wichita Falls?
A: “As of right now, zero. There was a rumor that the hospital had a case of COVID-19 and they weren’t telling anybody. If we get one, it is in everybody’s best interest that we tell everybody as soon as it’s confirmed so they’ll start washing their hands and doing what they should do.”
Q: Are we testing in Wichita Falls and how important is it to be tested?
A: “Yes and no. If you walked into my office from Italy and [you were coughing], I would say to call ahead and let us know you’re coming. At the door, we’re putting a mask on you and putting you back to a room where you will be alone. I’m going to put on my fancy suit with fomite protection, an N95 mask, eye protection and I’m going to go examine you. I’m going to test you for strep and flu; if both of those are negative I’m calling a friend of mine who is a county epidemiologist [who will tell me to] collect a nasal specimen and an oral specimen, put it in a viral transport medium, put it on ice and send it to the Public Health Department. The Public Health Department will put it on dry ice and send it to the nearest lab that is doing testing, which is Tarrant County and maybe Dallas. That’s how we get testing done. If you went to the hospital, the same thing would happen. Everybody is wired up about testing. The test is only important in epidemiology and public health. It does not change how we treat a patient or the outcomes. So once we’ve established if it is in the area and is circulating, there is no point in getting testing after that.”
Q: Is COVID-19 treated the same as the flu?
A: “It’s as treatable as a cold is. There is no treatment for a cold. [COVID-19] is a cold; now, it’s the bad sheep side of the family and it is the black seed, but it is a cold. It transmits the same way — through coughing and contact fomites, and there’s no specific treatment that is widely approved and there is no vaccine yet. Will those things come? Yeah, they will. Are they here yet? No, they are not. Most of the time it’s going to be a cold. Here’s my explanation to make it accessible: 100 people get COVID-19. Two weeks later, 85 [of them] are going to say ‘That wasn’t so bad, I’ve had a cold like that before,’ another 10 of those are going to say ‘That was the worst chest cold ever! I thought I was going to die,’ but they didn’t. And another five of those are going to need hospitalization, and of those, three are going to need intensive care, but there are only going to be two beds left [in the hospital] and of the two that get intensive care, they’re both going to need a ventilator and there’s only going to be one left — that’s where the problem is. There are not enough resources. Hospitals are very expensive to maintain empty, so we don’t have excess capacity. We have just enough — we can barely get through the flu season every year — and this has an order magnitude of a higher case fatality rate than the flu. [Even if we did have an ample amount of resources] people still die. It just gets that bad sometimes.”
Q: How can we stay healthy over spring break?
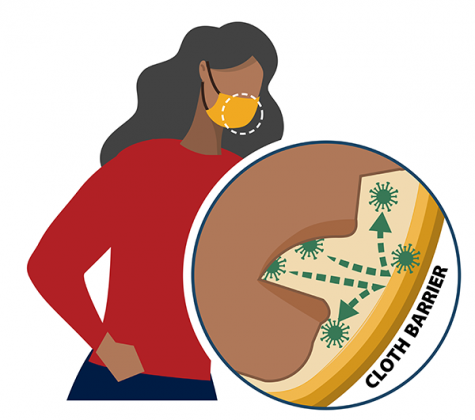
A: “Basic prevention falls into two phases — prevention of contact and staying healthy. Prevention of contact is simply washing your hands because who knows who touched that doorknob last or that keyboard last; if someone is coughing, stay six feet away from them [because] fomite respiratory cough droplets will travel about three to three and a half feet; and if you get sick, cover your cough in your sleeve, preferably not your hands because [you touch things with your hands] or cover it with a kleenex and throw that away, and that would be an appropriate time, if you have a persistent cough, to wear a mask to prevent yourself from spreading it to people. The other half is improving your immune system. You sleep properly, eight hours a night, preferably the same hours every night — that has to be practiced to get it right. Eat well [and keep] a balanced diet — nothing too fancy. Exercise. Now, don’t kill yourself trying to become the next Iron Man triathlete, but exercise improves immune function.”
Q: What are the signs and symptoms of COVID-19?
A: “Viral illnesses have classic three-phase presentation; Asthenia – ‘I don’t feel right,’ Qatar – ‘I have a sore throat, fever, body aches and nodes,’ Paroxysm – the cough. They typically occur in that order. With the flu, it hits like a ton of bricks. Coronavirus is more insidious; it grows gradually over the first week and the second week seems to be the hard week.”
Q: Should we be freaked out?
A: “To an adequate and proportional level. You should be freaked out enough to wash your hands and do all that proper stuff, but you shouldn’t stop doing things and living your life until it becomes the right thing to do because you’re helping the community limit the effect of the virus.”
Q: Is there a demographic of people who are more at risk?
A: “It prefers the elderly and infirm, particularly those with heart disease, lung disease and diabetes. There are instances where perfectly, otherwise reasonably, healthy 34-year-olds get severe form. The good news is, for whatever reason, it is extremely uncommon for those less than age seven.”
Q: Because of President Trump’s 30-day ban on European travel, how does this affect international students?
A: “We will learn that as we go. Midwestern instituted a travel recommendation to cancel all travel to level 2 or 3 places, and if you go there on your own, you should self-quarantine or self-isolate, which is what I’ve heard on all the national news like the rest of the people; that is what is being recommended if you’re returning from Europe.”

Kristin Silva is the former Chief Editor at The Wichitan.
She began her journey in Spring 2018 as a reporter who dabbled in photography for a short...